Wait Times Aren’t Longer in Countries With Universal Healthcare
What I learned about healthcare from my time in Iceland and Greece
In late 2022, I traveled outside the United States for the first time. After spending almost all my life living in Los Angeles, Florida, Arizona, and other areas around the hot Southern United States, it was time for a change. I skipped the tropical islands of the Caribbean for something different.
Palm trees and sunny beaches get humdrum after a while. I wanted a change of pace. I wanted to go to the coldest, darkest island I could find in mid-December. My girlfriend and I picked Iceland.
I was dealing with a severe back injury — three compressed vertebrae, C3-C5. The flight across the Atlantic was simultaneously brutal and exciting. I constantly winced in pain as I was forced to sit upright in the airline seat. Sleeping wasn’t remotely in the cards.
Any time I laid down or sat upright, any time my spine was straight, I felt a stream of ruthless pain traverse my body. Anyone who’s dealt with a spine injury knows how ravaging the pain can be.
Still, Iceland was phenomenal. Stunning landscapes, friendly people, and the beautiful cold darkness I had set out for, all greeted me at every turn. We bathed in the volcanic hot springs and pounded the pavements of Reykjavík, the capital city.



I started asking the locals about the healthcare system in case I needed to do something about the searing pain shooting up my spine, preventing me from sleeping throughout the trip.
Everyone explained to me that if I wanted to be treated for my back issue — even as an American — all I needed to do was go to the hospital and I would be seen for free or next to nothing. They said it might take me anywhere from a few hours to a half of a day to be seen since my injury wasn’t life-threatening. But, I would be seen.
Since we didn’t have that long in Iceland, I decided to skip the hospital and bite through the pain. But I took note of the option of being seen the same day at the hospital for free or near-free in Europe.
Almost one year after Iceland, I felt the familiar pang of wanderlust again. After five long years of work-from-home, I was itching to get out and see more of the world.
I packed my bags and set my sights on Europe once more, this time spending three months in Greece. This trip, too, was enthralling. I went to Athens for two months, spent a week in Crete, and then the rest of the time back in Athens again.
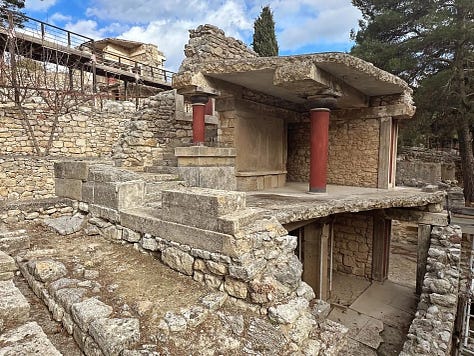
While in Crete, I visited the Minoan palace at Knossos, which began construction in 1,900 BCE, near Heraklion. Knossos itself was settled around 7,000 BCE. I nearly had an existential crisis, standing on 9,000 years of civilization and trying to visualize the distant past and the innumerable people who lived there.




I left my medications back in the United States, unsure if it’d be legal to bring them into Greece, and decided to visit a doctor upon arrival instead. I contacted a family doctor in Athens and told him I was dealing with insomnia thanks to the jet lag from the long flight. He kindly informed me that I needed to speak to a psychiatrist before scheduling my appointment.
My friend sent me a website where I can book appointments with doctors in a range of fields. I booked an appointment that same day and saw a psychiatrist that afternoon in person. I was astonished. I saw two specialists across three visits — a psychiatrist twice and a neurologist once — all same-day visits.
The cost of each visit was €50 and the medication I was prescribed for the jet lag cost €1.90 for a two-month supply. I checked GoodRx for the same medication to see what it would’ve cost me in the U.S. for the same amount, and it was $88.40. I was paying $36 per month for a similar medication back home. Stunned, I took a picture.
But the real shock didn’t happen until I flew home. Once I arrived back in the US for Christmas, I tried to set up an appointment with my doctor to go over some simple blood work. The wait is four months to see my doctor in person.
This belies a myth about our expensive privatized healthcare system: that it’s superior to other systems because you get what you pay for. Surprised by these two travel experiences (more like revelations), I started digging to see what I could find about healthcare wait times.
Over the years, I’ve heard repeatedly that medical wait times in the United States are significantly shorter than those in countries with public healthcare systems, like Canada, the Netherlands, or Germany. The benefit of having a private healthcare system, proponents argue, is shorter wait times and better care. You know the mantra.
Politically minded think tanks have pushed the message (here and here) that universal or publicly funded healthcare necessarily leads to longer wait times. Senator Ted Cruz of Texas can be seen peddling this tale here. But is it true?
Let’s Talk About Wait Times
Whenever I had discussions about this in the past, I intuitively knew there was a disconnect between how healthcare is financed and healthcare wait times. Healthcare and healthcare finance are two different things. If there’s a shortage of doctors, it matters not whether public or private money pays them.
As far back as 2013, The Commonwealth Fund found, of healthcare wait times, America had the third-longest wait times behind Canada and Norway. This is not a new phenomenon.
The survey was composed of 20,045 adults in eleven countries, 2,002 of them from America. This is a pretty massive data set. It was subsequently reported by Elisabeth Rosenthal in the New York Times the following year, in 2014, in a piece that began questioning the long-held American dogma that the high cost of our healthcare is the price of short wait times.
In 2016, the OECD found that the United States had surpassed Norway and taken second place behind Canada. Updated data in 2020 found things haven’t changed much. Canada is in first place for the longest wait times, with the United States in second, and Canada still has a better healthcare ranking than the United States overall because it isn’t obscenely expensive.

High wait times in America are especially true when seeing a primary care doctor. As of 2023, the United States has the longest wait time to see a primary care physician, with the average wait time being three weeks.
To be fair, the U.S. does pretty well with elective surgeries, according to a meta-analysis by Daniel McIntyre and Clara Chow. But, the researchers didn’t include the wait to see your primary care doctor to get the referral you need to have the elective surgery in the first place. In America, you usually need a referral from your primary doctor to see a specialist, at least if you want your insurance or Medicare to cover it.
Also, the United States fared a lot better regarding a specialist where the United States was in eighth place (for the longest wait time) behind the Netherlands, Germany, and Switzerland (whose system is quite like ours). The takeaway is pretty clear: paying more for the red carpet service of a fully privatized system doesn’t guarantee shorter wait times. It’s more of a mixed bag, independent of whether the system is publicly or privately funded, universal or partial.
The disconnect I’d always felt intuitively is confirmed.
A 2022 report from AMN/Merritt Hawkins found the average wait time for a doctor’s appointment in 15 of the largest metropolitan areas in the U.S. was 26 days. This is 24% higher than it was in 2004 when the physician survey was first conducted.
My four-month wait is extremely long compared to the twenty-six-day average, but it’s still not great. Call me crazy, but I think twenty-six days is a very long time to wait when you have a health problem. And it’s certainly longer than the same-day appointments I was getting in Greece and told about in Iceland.
I’m currently in Florida where there’s a shortage of doctors and nurses throughout the state. That shortage is poised to get worse and it debunks the idea that the private market will magically solve the problems of healthcare wait times.
But what does this mean for everyday Americans like myself?
Patient delays can result in worse care and raise the risk of mortality significantly. It should be a no-brainer that if you have a lot of people stuck in a triage awaiting care or riding out illness or injury at home, it’s going to negatively impact the health outcomes of many of those people.
Research by Simon Jones et al., published in the Emergency Medicine Journal, compared the health outcomes of 26,738,514 people who received emergency treatment and found that patients had an 8% higher risk of dying if they waited between six and eight hours to receive treatment at the ER.
Now, in case you’re thinking it’s COVID-19 driving these findings, guess again. The research was conducted between 2016 and 2018, several years before the pandemic reached American shores. Chances are, it’s only gotten worse since, as “COVID burnout hitting all levels of [the] healthcare workforce,” according to the Harvard Gazette.
Other research found that every month cancer treatment was delayed the risk of death rose by 10%. Of course, cancer treatment requires proactive citizens to get the checkups they need, which is hard for many people to do as it’s cost-prohibitive.
This brings me to another complication plaguing American healthcare: People are postponing necessary and often preventative care because they don’t want to deal with the cost burden. Last year, PBS reported:
Nearly a third of Americans lack access to primary care services, including routine checkups, while 40 percent of U.S. adults say they’re delaying care or going without because of the financial costs.
That 40% number tracks with a Gallop poll that found that 38% of U.S. adults put off medical care in 2022. In other words, Americans wait longer for care while a significant number of health concerns aren’t receiving care at all. Meanwhile, healthcare spending per capita and as a percentage of GDP remain stubbornly high despite not everyone being covered and many who are covered, aren’t seeing the doctor when they need to.
Our private system is supposed to be the fast track to seeing a physician, but it underperforms under less strain than the universal systems of Europe. My experience confirms this and proves that just because our system is private doesn’t mean we have shorter wait times.
My question is: when are we going to start demanding more?
In the meanwhile, I don’t mind taking a trip to Athens or Istanbul to get a little healthcare with my vacation.






